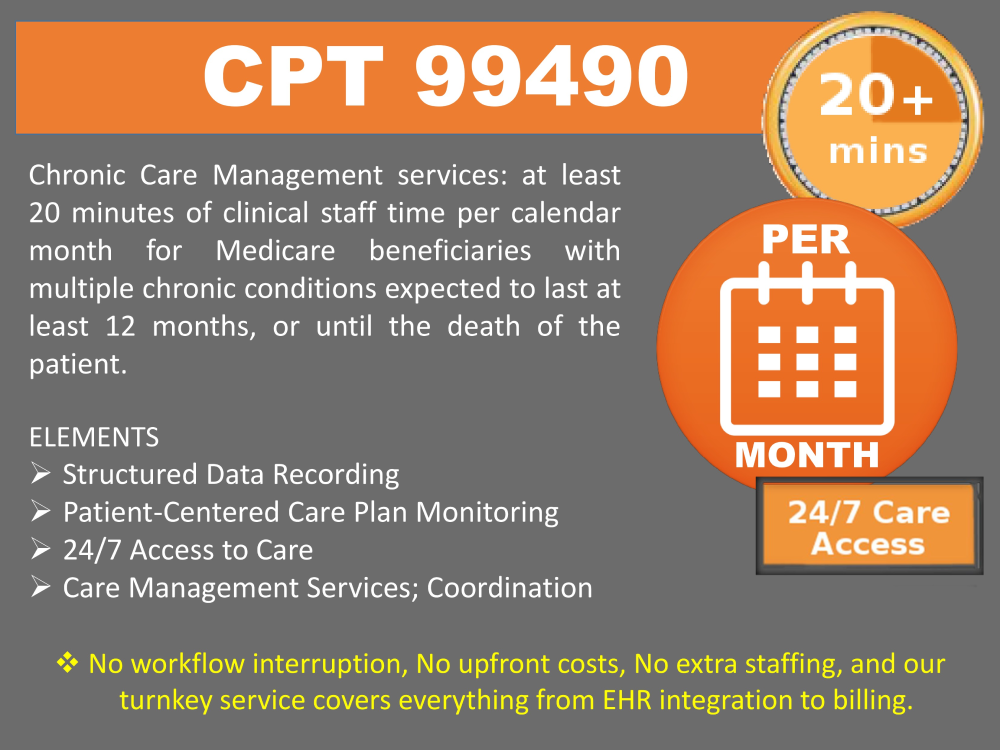
Chronic Care Management CPT 99490
What Is Chronic Care Management?
The Centers for Medicare & Medicaid Services (CMS) recognizes care management as a critical component of primary care that contributes to better health and reduced spending.
Beginning January 1, 2015, Medicare pays separately under the Medicare Physician Fee Schedule (PFS) under American Medical Association Current Procedural Terminology (CPT) code 99490, for non-face-to-face care coordination services furnished to Medicare beneficiaries with multiple (2 or more) chronic conditions.
*CPT 99490 copyright 2014 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. For a summary on the Medicare Learning Network® (MLN), refer to the “Medicare Learning Network® Catalog of Products” located at http://www.cms.gov/Outreach-and-Education/
CCM Scope of Service Elements - Highlights
Structured Data Recording
Care Plan
Access to Care
Manage Care
Care management services such as:
Chronic Care Program Highlights
Patient-Centered
Implement and monitor - and revise as needed - provider-guided care plan using clinical, behavioral, and educational measures.
Identify Barriers
By identifying barriers, we develop positive health outcomes by addressing healthcare behaviors in both patients and provider.
Care Coordination
Address communication barriers between care providers and patients utilizing specific behavioral, clinical, and educational principles to encourage change.
Medication Reconciliation
Medication reconciliation with review of adherence and any interactions; and oversight of patient self-management of medications.
24/7 Care
Anytime access will support patient’s around the clock - with full EMR including documentation of their progress.
Our Engagement Measures 4-level engagement measure
Using a series of progressive assessment measures, activities, and surveys, our care team will determine each patient's level of engagement with their healthcare and determine a course of training. The 4 levels include:
Level 1
- Disengaged.
- Individuals are passive and lack confidence.
- Health knowledge is low.
- Goal orientation is weak.
- Adherence is poor.
- Their perspective: “My doctor is in charge of my health.”
Level 2
- Becoming aware but still struggling.
- Individuals have some knowledge, but large gaps remain.
- They believe health is largely out of their control, but can set simple goals.
- Their perspective: “I could be doing more.”
Level 3
- Taking action.
- Individuals have the key facts and are building self-management skills.
- They strive for best practice behaviors and are goal-oriented.
- Their perspective: “I’m part of my health care team.”
Level 4
- Maintaining behaviors and pushing further.
- Individuals have adopted new behaviors but may struggle in times of stress or change.
- Maintaining a healthy lifestyle is a key focus.
- Their perspective: “I’m my own advocate.”
Our Core Features
Software
Award-winning platform, gold-standard apps, EHR integration.
Staffing
Expand your care team to reach patients beyond your daily schedule.
24/7 Care
Care centers are staffed for your patients, under your orders; supervision.
Compliance
Fits ACA measures, HIPAA compliant portals, EHR integration.
